Think back to your last doctor’s visit; you most likely spent the first minute of the appointment filling in the provider with up-to-date health information, perhaps even referencing your wearable device info to provide more context. If you have a chronic illness, you most likely spent time bringing to light recent changes in your health based on ongoing treatment. If you are a care provider for a loved one, you may have a notebook or try to use your spotty memory to fill in the patient profile to assist the physician in defining a care plan.
In this context, as a patient or caregiver, you act as the database for your personal health information. You are the information interface to the provider’s Electronic Health Record (EHR) system, bringing external information and context to the provider to enrich your patient profile and ultimately helping to set the course for a personalized care plan. This is good as you are taking accountability for your health. However, in the infamous words of the Six Million Dollar Man, “We have the technology!” We must ask why we are not leveraging technology to bridge this information gap.
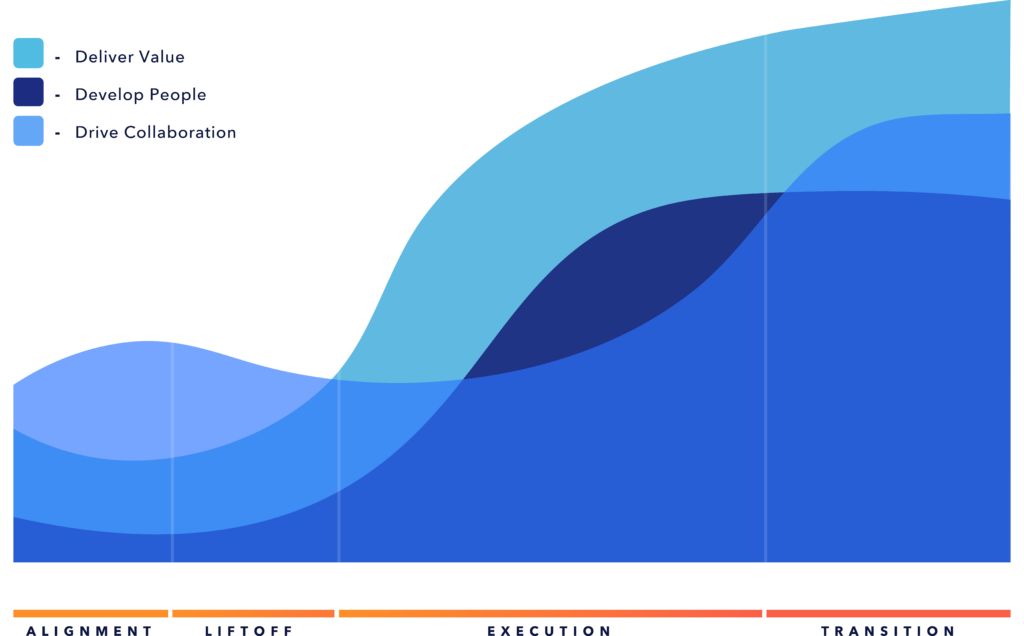
The role of patient data in driving value-based care
In the current paradigm of the US healthcare system, healthcare institutions are not effectively leveraging the growing, robust landscape of personal health data captured outside of the provider system, ultimately creating barriers to developing personalized care models and implementing value-based care. The patient profile being shared is incomplete and neglects large segments of a patient profile, including caregiver data, data captured from commercial devices, digital therapeutics, home health medications, and detailed genetic history. The data in the EHRs is point-in-time and incomplete, resulting in less-than-optimal patient outcomes.
To bridge this gap, the strategy has been to develop standalone Personal Health Databases by tying into EHRs at the institutions and then attempting to capture commercial device data, imaging, and unstructured care data into a standalone model. The challenge with this approach is that the data lays dormant in the standalone data framework with no bi-directional data exchange, essentially creating more headaches for the patient and the provider, with the only integration point being a voice-over from the patient at the time of the clinical interaction. The other approach has been to develop a health system-based patient data hub that tracks the multi-modal clinical data captured within the health system and allows patients to upload certain data elements manually. This is moderately effective if the patient can keep all encounters within the system and integrate other data diligently. It is not easy. Both approaches fall woefully short of providing a complete patient health record and real-time data for clinical decision-making.
Making the shift
Inevitably, poor patient outcomes, revenue challenges, changing population demographics, and regulatory pressure will drive a profound change in the orientation of personal health data management. It is not a stretch to believe that, shortly, we will see a shift from institutional ownership to patient-owned data that will enable individuals to capture, store, secure, share, analyze, and monetize their health data through the value chain.
Shifting the orientation of the data ownership model from the institutions to the individual will help unlock the potential of personalized medicine and improve patient outcomes. Individuals are the stewards of their health data. They are ultimately incentivized by health plans to be more accountable for outcomes and solidify the linkage between value-based care and personalized medicine.
Changing generations will be the primary driver for the paradigm shift to patient-owned data that will enable the patient-facing health economy. As the more tech-oriented generations become the primary users of the system, there will be an expectation of tech-oriented customer service manifested through data. Also, as the landscape of personal health data grows outside the walls of the institution, the need to enrich the patient profile with personal health data captured through commercial devices will be expected.
This disruption will force structural changes to the regulatory environment, technology strategies, core operating models, clinical decision-making frameworks, and healthcare investment perspectives in the healthcare ecosystem.
Seeking better patient outcomes
The US healthcare system is gradually shifting from the current Fee-for-Service model to a Value-Based Care (VBC) model, which is predicated on the value provided to the patient and better patient outcomes. Centers for Medicare & Medicaid Services (CMS) plans to enroll all Medicare and Medicaid beneficiaries in value-based care programs by 2030. While private programs will take longer to enroll, as the currently defined VBC model leaves gaps in the care model and puts increased financial stress on already stretched institutions, they will eventually be driven to an outcome-based model.
The core charter for value-based care is to improve patient outcomes, improve patient experience, and address equity/access issues, ultimately aiming to reduce the cost of care. The objectives of the new accountability model are still controversial and have yet to be fully adopted by most health systems. As the march towards VBC continues, it brings to light the need for personalized care, which is at the heart of the accountability model. The focus on the patient outcome is the focus versus charge by service code for revenue generation.
The movement to personalized care places personal health data at the center of the care journey.
A key component of the success of value-based care will be the growth of personalized medicine, which will drive the development of individualized, efficient care models, ultimately improving outcomes and reducing the cost of treatment. The movement to personalized care places personal health data at the center of the care journey. The ability to capture and integrate personal health data into the clinical decision-making framework is a critical first step to developing efficient, personalized treatment plans.
The role of regulation
In 2020, the Department of Health and Human Services (HHS) mandated the 21st Century Cures Act and the MyHealthEData initiative to drive the CMS Value-based Care implementation. At the core of the rulings is the charter to allow patients to access their health data to enable price transparency and drive accountability for their care decisions. Similar regulations have been implemented in the EU (article 15 GDPR) and portability (article 20 GDPR), emphasizing data access and portability. Although regulatory steps are being taken to push these critical initiatives, the impact has yet to be felt at the patient level.
Despite the best efforts of healthcare institutions, patient experience and patient engagement continues to be a challenge. In the current paradigm, the patient is caught in a whirlwind of multiple provider engagements, and access to personal health data is exposed by a labyrinth of fragmented access portals, resulting in a huge degree of frustration.
Although the regulations open the doors to breaking the institutional monopoly on health data, it has done little to move the needle. This could be perceived as being purposeful. As a patient, the less you know about services, charges, and data exchanges between providers, payers, and pharma companies, the institutions remain in the driver’s seat. Personal health data is leveraged as a control mechanism, making the fee-for-service model opaque to the user or patient.
Changing patient behavior
The formula is simple: If we have the data, we can develop insights. If we can develop insights, we can change behavior. If we change behavior, we can improve outcomes.
To change the current care paradigm and drive to value-based care, it will be critical to change the perspective on health data management. Instead of point-in-time data capture, managing personal health data should be viewed in the context of a real-time, continuous monitoring framework leveraging data captured inside and outside of the facility. A system based on 24-hour patient monitoring for both healthy and ill patients that is responsive to data captured in real time.
We have many ways to capture health data, but currently, there is no way to consolidate all the data and effectively drive changes in behavior using data. On our own, we are capturing health data through multiple commercial Internet of Things (IoT) devices that provide 24/ monitoring capability, such as fitness bands, health trackers, blood pressure monitors, sleep monitors, etc. We also go to the gym, ride bikes, take walks, and our spouses recognize changes that may elude us. In the current system, this enriched data has little to no bearing on the clinical decisions made by the providers due to the lack of integration. There is no mechanism to consolidate data outside the facility with data inside the facility, resulting in a healthcare system predicated on point-in-time, generalized care models.
The fragmented, reactive model starts with collected health data scattered through a landscape of disparate sources. The institutional data is incomplete and generally inaccessible to patients unless they use a third-party service to leverage the APIs provided by the hospital to access their data. Last time I checked, my 75-year-old mother was not a programmer who would tap into a set of APIs to get her latest scan results; thus, the patient data is lost in a sea of institutional databases and accessible through a web of individual portals. The data outside of the facility sits in commercial databases fronted by IoT devices and companion applications. The result is a tangled mess of data that does not serve the patient in a cohesive, singular experience.
To prepare participants throughout the healthcare value chain for patient-owned data or the “Personal Health Hub” concept, Industry leaders must begin to reimagine healthcare interoperability and data management as a robust fabric of tightly managed, secure, bi-directional, data exchanges between healthcare institutions, patients, commercial entities, and clearing houses at a national scale.
In contrast to a landscape of disparate data sources housed by institutions and exposed by various portals, in the future, personal health data will be owned and managed by the patient and fully integrated into clinical decision-making frameworks, opening the door to B2B and B2C integration models.
Preparing for patient-owned data
From payers, providers, pharma companies, and all the participants in between, institutions must be prepared for the shift to patient-owned data. Shifting the orientation of data to the patient will enable the patient to secure and perhaps monetize their data in the future, which will completely disrupt current operations, investment strategies, and data governance policies.
To mitigate downside risk, leaders must “skate to where the puck is going” and think about shifting long-term investment bets to:
- Consumer-based healthcare enablement
- Innovating personalized medicine leveraging enriched patient data
- Enhanced data management frameworks and tooling to regulate ‘patient-owned’ data in the ecosystem.
- Revision of compliance and regulatory policies
Navigating the change of patient-owned data will not be easy, but institutions must begin the journey now. The regulations being put in place are acting as beacons to the coming changes in health data access, patient rights, data security, and interoperability.