The Evolution of the Doctor-Patient Relationship in the Age of AI
In the rapidly advancing landscape of healthcare technology, perhaps no development holds more transformative potential than the integration of generative and agentic artificial intelligence into the doctor-patient relationship. This foundational relationship, built upon centuries of evolving medical practice, now stands at a crossroads as AI systems increasingly participate in diagnosis, treatment planning, and even direct patient communication. This article explores how AI is and will continue to fundamentally transform the doctor-patient relationship.
The traditional doctor-patient dynamic
The doctor-patient relationship has historically been characterized by an inherent power imbalance. Physicians possess specialized knowledge gained through years of rigorous training and clinical experience, while patients frequently arrive in states of vulnerability, seeking expertise they themselves lack. This dynamic has evolved over decades from a paternalistic model where “doctor knows best” toward more collaborative approaches emphasizing shared decision-making and patient autonomy.
Even in its most modern, progressive forms, this relationship rests upon distinctly human foundations: empathy, intuition, cultural context, and the ability to navigate emotional nuance. These elements form the bedrock of trust that enables effective healthcare delivery.
AI as the third participant in the examination room
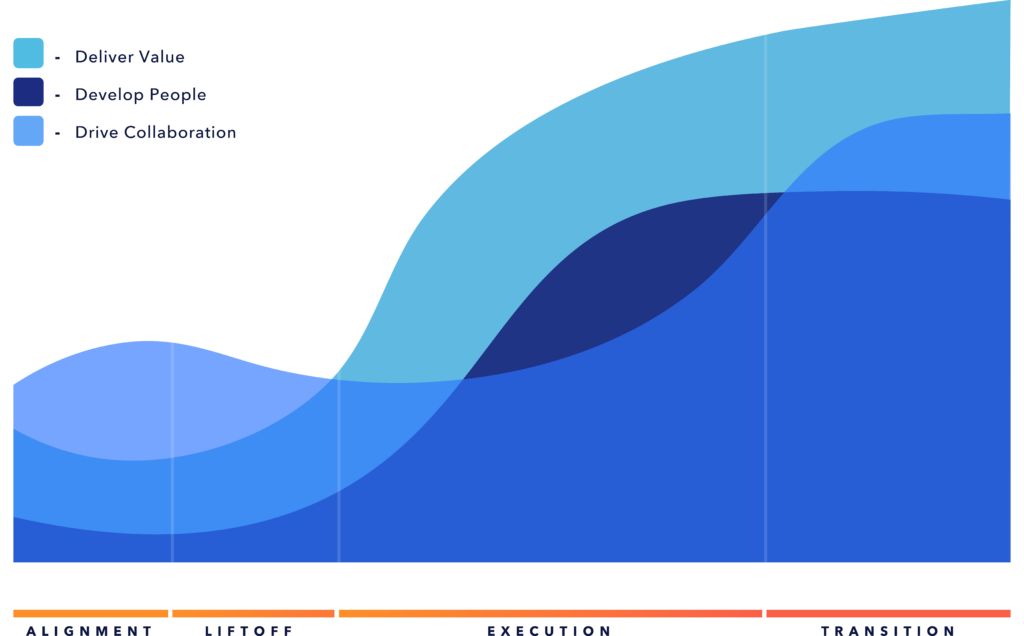
The introduction of sophisticated AI systems fundamentally transforms this dyadic relationship into a triadic one. AI algorithms are already participating in diagnostic processes, treatment planning, risk assessment, and care coordination. As these systems advance, their roles will inevitably expand, raising profound questions about how their presence reshapes the doctor-patient interaction.
When an AI system flags a concerning pattern in a mammogram that a radiologist might have missed, or when an algorithm suggests an alternative treatment protocol based on analyzing thousands of similar cases, the physician becomes both interpreter of AI outputs and medical authority in their own right. Patients, meanwhile, must navigate trust not only in their human provider but also in the invisible algorithmic processes influencing their care.
Another potential for profound change in the doctor-patient relationship is the examination room. The examination room will become less a place of discovery and more a space for trust-building, conversation, and decision-making about treatment options already generated through the AI-driven analysis of patient data. AI-powered healthcare technologies are starting to challenge the centuries-old paradigm that diagnosis must occur in the physical examination room, or more recently, through telehealth. In the near future, wearable sensors, remote monitoring systems, smart clothing, smart(er) apps, and home digital therapeutic and diagnostic devices will make it possible for both doctors and patients to come to appointments with unprecedented information about possible diagnoses and treatment options. These will allow continuous monitoring of patients’ health parameters outside traditional medical settings, with AI systems analyzing the data for disease prediction and diagnosis while providing possible treatment guidance before the patient even steps into the doctor’s office.
Similarly, AI might serve as a democratizing force, reducing the knowledge asymmetry that often characterizes medical encounters. Patients equipped with AI-powered health assistants could arrive better informed about their conditions, enhancing their capacity for truly shared decision-making. For physicians, AI systems offering real-time guidance might enable more compassionate and personalized care by freeing cognitive resources previously devoted to reading copious clinical notes in EHRs and recall of medical facts.
Challenges to trust, transparency, and connection in AI-powered care
Yet considerable challenges accompany these potential benefits. The “black box” nature of many AI systems threatens transparency in medical decision-making. When neither physician nor patient fully understands how an AI reached a particular recommendation, the foundation of informed consent becomes precarious, and prone to litigation.
Additionally, over-reliance on AI systems risks diminishing the human connection at the heart of healing relationships. Medical decisions often involve complex value judgments that extend beyond clinical parameters. The physician who knows a patient’s life circumstances, values, and preferences brings contextual understanding that even the most sophisticated AI may struggle to incorporate.
Reimagining medical education and practice
As AI increasingly handles certain aspects of diagnosis and treatment planning traditionally performed by physicians, medical education must evolve accordingly. Tomorrow’s doctors will need training not only in clinical medicine but also in effectively collaborating with AI systems, critically evaluating algorithmic outputs, and communicating AI-derived insights to patients in accessible ways. The clinical encounter itself may require restructuring to accommodate AI’s presence. New protocols, such as introducing AI participation to patients, explaining algorithm-derived recommendations, and managing disagreements between human and machine judgments, will become essential elements of care delivery.
Overcoming cultural resistance to AI in healthcare
Cultural attitudes toward AI in healthcare will significantly influence its integration into the doctor-patient relationship. Some patients, particularly younger generations and those with technological affinity, may readily embrace AI participation, while others may resist what they perceive as technological intrusion into a deeply personal domain. These attitudes will likely vary across cultural contexts, socioeconomic groups, and geographic regions, raising the risk of a “two-tier” system in which some patients benefit from advanced AI while others receive traditional care potentially exacerbating existing healthcare disparities.
Balancing trust and data ownership in AI-driven healthcare
The introduction of AI in the doctor-patient relationship creates a fundamental tension between potential benefits and privacy concerns. Patients recognize the value of sharing data from wearables and home monitoring yet hesitate due to uncertainty about who controls this information. Unlike the traditional model where health data remained within clear doctor-patient boundaries in EHR systems, today’s digital ecosystem involves multiple entities accessing and potentially monetizing intimate health information. High-profile privacy failures in AI implementations have only reinforced patient wariness about sharing their data.
Resolving this paradox requires more than technical solutions. It demands a fundamental reimagining of data governance in healthcare. Successful AI implementation will depend on creating frameworks that acknowledge patients as the rightful owners of their data while providing transparent processes for how that data will be used, shared, and protected. When patients understand not just how their data might improve their individual care but also how their privacy will be safeguarded, the trust essential to AI adoption can flourish. Only by addressing both the ownership question and the trust deficit can we unlock the full potential of AI-augmented healthcare while preserving the human-centered values at medicine’s core.
Beyond technology: the ethics of AI in the doctor-patient relationship
The integration of generative and agentic AI into healthcare represents not merely a technological shift but a profound reimagining of one of society’s most essential relationships. How we navigate this transformation will determine whether AI becomes a force that enhances the human dimensions of medicine or one that diminishes them. By approaching this evolution thoughtfully with careful attention to questions of trust, transparency, equity, and human connection, we have the opportunity to preserve what is most valuable in the traditional doctor-patient relationship while addressing its limitations through technological innovation.
To learn how your organization can responsibly integrate AI into patient care while upholding human-centered values, connect with our team or explore our healthcare transformation insights.